Personalized Risk Calculator for Esophageal Adenocarcinoma
Intended audience
This tool was designed for use by health providers with their patients. Please take these results to your health provider to discuss your personal risk of esophageal adenocarcinoma. IC-RISC™ (“Interactive & Contextual RISk Calculator”) currently applies only to white males, black males and white females, which are the groups with the most accurate information on incidence and risk factors. The incidence of EA is very low in black females, and little risk factor information is available specifically for Hispanics or persons of other ethnic/racial backgrounds.
Background
Esophageal adenocarcinoma (EA) is an aggressive cancer usually arising in the lower part of the esophagus near the stomach. Once quite rare, its incidence has risen substantially over the past four decades in the U.S. and many other developed countries. It is most common among white males, although incidence rates in other groups also have risen. Unless diagnosed at an early stage, long term survival with EA remains poor. Therefore preventing the cancer and detecting it at an early stage remain the most effective options.
Purpose
Epidemiologic and clinical research has revealed many risk factors which, taken together, can help estimate a person's probability of developing this cancer. These include demographic factors, host and lifestyle factors, medications, family history, and genetic markers. IC-RISC™ uses an individual's risk factor profile to estimate his/her absolute risk of developing EA over the next ten years. While incidence of this cancer has increased, it is still relatively rare. To put this in perspective, risk of developing EA is displayed in the context of risk of dying from other cancers or from causes such as injury, stroke or heart disease. In this way the tool can help inform discussions between a health provider and patient regarding:
- how personal risk of EA fits into the “bigger picture” of health and disease,
- whether preventive actions are indicated to possibly reduce risk of EA and other conditions, and
- whether additional tests and procedures might be warranted to identify and manage those with high risk profiles.
Use
Enter values for risk and preventive factors on the left side of page, Separate tabs are available to aid in calculating BMI and categorizing usual physical activity. The estimated 10-yr probability of developing EA is displayed on the right side in two ways:
- a “thermometer” with color coded risk (on a log scale), along with an estimate of its uncertainty, and
- a set of 1,000 circles depicting the expected number who will (red fill) and will not (unfilled) develop the cancer in the next ten years.
Disclaimer
This application should not be considered, or used as a substitute for, medical advice, diagnosis or treatment. This site does not constitute the practice of any medical, nursing or other professional health care advice, diagnosis or treatment.
Note: Disease incidence and mortality rates used in IC-RISC™ are specific for the U.S.; comparison mortality rates are specific for age, sex and race, but do not take into account other risk factors.
Click blue buttons for more information
Calculate Body Mass Index (BMI)
More information on BMI and health can be found at
Centers for Disease Control
and
National Institutes of Health
Calculate Physical Activity Category
Moderate physical activity per week
Vigorous physical activity per week
Risk factors by Barrett's status
Parameter Values - BE negative
Parameter Values - BE positive
Change Log
Version 1.1 (17 Jun 2019)
- Release version for publication (BMC Gastroenterology, 2019) (https://ic-risc.esocan.org)
Version 1.01 (5 Dec 2018)
- Release version for website (https://ic-risc.esocan.org)
- Updated license
Version 1.0 (20 Oct 2018)
- EAC incidence in BE positive white men reduced from 0.42 to 0.31% per year
- EAC incidence in BE positive white women reduced from 0.5 to 0.4 rate in white men
- EAC incidence in BE positive black men reduced from 1.0 to 0.75 rate in white men
Version 0.9.0.1 (30 Sep 2018)
- Updated relative risk for NSAIDs, statins and reflux
Version 0.8.1 (22 Aug 2018)
- Added licensing information
- Minor organizational changes
Version 0.8.0 (2 Aug 2018)
- Changed SEER comparison to 2018 release of SEER18
- Added possibility of two or more family members with BE/EA
- Updated population prevalence for several risk factors
Version 0.7.4 (8 Jun 2018)
- Modified overall BE progression rates to weight LGD and HGD using relative risks of 3.68 and 20.0.
Version 0.7.3 (4 Jun 2018)
- Improved help popups
- Modified biopsy prevalence based on CISNET assumptions
Version 0.7.2 (10 May 2018)
- added screen-negative effect to calculator (SIM-negative stratum(
- added reflux to SIM-positive stratum
Version 0.7.1 (30 April 2018)
- added low-grade dysplasia to risk calculator
- updates to documentation, relative risks and references
- correction applied to incidence among SIM-positive (Barrett's) persons
Version 0.7.0 (16 Aug 2017)
- all risk projections are now for 10 years rather than 5 years
- all comparison rates are now mortality-based rather than a mix of incidence and mortality. For cancers with good survival (e.g., prostate, colon) the comparison rates will therefore be substantially lower
- EA rates have been updated to latest SEER release (2010 - 2015 diagnosis years)
- New menus separate risk factor information from other information
Version 0.6.1 (2 june 2017)
- confidence interval now takes into account uncertainty in calculating baseline hazard (via PAF) as well as an invidual's relative risk
Version 0.6.0 (5 may 2017)
- calculator now includes rates and risks for black males and white females (rates among black females is extremely low)
- incidence and mortality rates for comparison diseases have been updated to most recent available
- all comparison rates are now specific for age/sex/race group
- additional menu items have been added and consolidated uner “more information”
- risk factor information (relative risk and confidence interval) are now presented graphically
- EA incidence and overall mortality graphs are available by age/sex/race
Version 0.5.3 (21 feb 2017)
- color and numeric scales are now identical for SIM-positive and SIM-negative
- added up/down arrows for situations where estimated risk is beyond scale
- filling of circles for dot plot now begins in upper left
Version 0.5.2 (7 feb 2017)
- added confidence band (preliminary calculation)
- modified default smoking status to “ever smoker”
Version 0.5.1 (7 dec 2016)
- changed color of SIM-positive thermometer to match SIM-negative, but extend to brighter yellows
- added statins to prevention section
- changed “clinical” wording to “screening results”
- use negative/positive/unknown as options for SIM status (currently SIM negative and SIM unknown yield same result - this is under review)
- change default SIM segment length from zero cm to 2 cm
Version 0.5.0 (5 nov 2016)
- modified calculation of 5-year esophageal adenocarcinoma incidence to account for competing risks (as per Gail, 1989)
- changed appearance of thermometer and risk marker (for simplicity)
Version 0.4.2 (29 sep 2016)
- converted smoking pack-years to ever/never (for simplicity)
- rearranged groups of factors
- added physical acivity calculator
Version 0.4.1 (15 sep 2016)
- added progress bar
- added footnotes to thermometer
Version 0.4.0 (14 sep 2016)
- added 3rd column for input data
- shortened thermometer to better fit on wide/short windows such as laptops
- added beginnings of help system
- added “what's new” tab
EAC incidence and overall mortality by age
License
License
Academic and non-profit use
IC-RISC software is made available for academic and other non-profit use under the 2-Clause BSD License:
Copyright 2019 Thomas L Vaughan
Redistribution and use in source and binary forms, with or without modification, are permitted provided that the following conditions are met:
Redistributions of source code must retain the above copyright notice, this list of conditions and the following disclaimer.
Redistributions in binary form must reproduce the above copyright notice, this list of conditions and the following disclaimer in the documentation and/or other materials provided with the distribution.
THIS SOFTWARE IS PROVIDED BY THE COPYRIGHT HOLDERS AND CONTRIBUTORS “AS IS” AND ANY EXPRESS OR IMPLIED WARRANTIES, INCLUDING, BUT NOT LIMITED TO, THE IMPLIED WARRANTIES OF MERCHANTABILITY AND FITNESS FOR A PARTICULAR PURPOSE ARE DISCLAIMED. IN NO EVENT SHALL THE COPYRIGHT HOLDER OR CONTRIBUTORS BE LIABLE FOR ANY DIRECT, INDIRECT, INCIDENTAL, SPECIAL, EXEMPLARY, OR CONSEQUENTIAL DAMAGES (INCLUDING, BUT NOT LIMITED TO, PROCUREMENT OF SUBSTITUTE GOODS OR SERVICES; LOSS OF USE, DATA, OR PROFITS; OR BUSINESS INTERRUPTION) HOWEVER CAUSED AND ON ANY THEORY OF LIABILITY, WHETHER IN CONTRACT, STRICT LIABILITY, OR TORT (INCLUDING NEGLIGENCE OR OTHERWISE) ARISING IN ANY WAY OUT OF THE USE OF THIS SOFTWARE, EVEN IF ADVISED OF THE POSSIBILITY OF SUCH DAMAGE.
Commercial use
IC-RISC software will be made available for commercial use under a negotiated license.
Contact
For academic and other non-profit use, download software at: https://github.com/FredHutch/IC-RISC-Working
For commercial use, contact Fred Hutchinson Cancer Center, Business Development & Strategy (206.667.4304)
Acknowledgements
Acknowledgments
There are many individuals who helped develop and shape IC-RISC™, and I am grateful to all. These include Lynn Onstad, James Dai and Li Hsu at Fred Hutch (http://fredhutch.org) who offered guidance and programming support for estimating risk and confidence intervals while accounting for competing mortality; Patty Galipeau, also at Fred Hutch, who suggested many usability improvements; and members of the BEACON consortium (http://beacon.tlvnet.net) and CISNET esophageal network (https://cisnet.cancer.gov/esophagus/) who offered helpful advice at multiple points during its development.
Contact
Please contact Dr. Thomas Vaughan with questions or suggestions at tvaughan (at) uw (dot) edu.
References
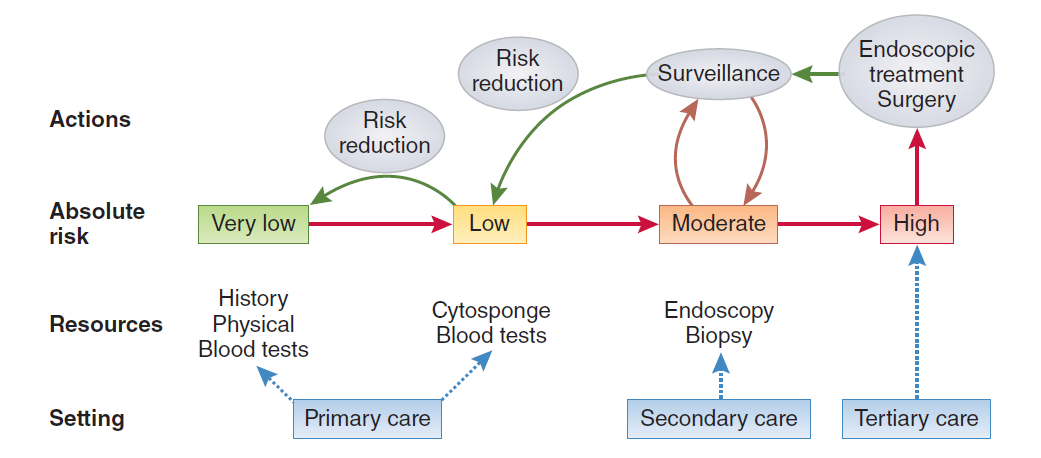
Additional information regarding how an esophageal cancer risk calculator and decision tool might be incorporated into clinical practice can be found in the figure (from ref #3) and following publications:
Thrift AP, Kendall BJ, Pandeya N, Whiteman DC. A Model to Determine Absolute Risk for Esophageal Adenocarcinoma. Clinical Gastroenterology and Hepatology 11, 138–144.e2 (2013).
Thrift AP and Whiteman DC. Can we really predict risk of cancer? Cancer Epidemiology 37, 349–52 (2013).
Vaughan TL. From genomics to diagnostics of esophageal adenocarcinoma. Nature Genetics. 46, 806-807 (2014). (See figure)
Rubenstein JH, et al. Prediction of Barrett’s esophagus among men. The American journal of gastroenterology 108, 353–62 (2013). http://mberet.umms.med.umich.edu/
Vaughan TL and Fitzgerald RC. Precision prevention of oesophageal adenocarcinoma. Nature Reviews Gastroenterol Hepatol 12, 243-48 (2015).
Xie S-H, Lagergren, J. A Model for Predicting Individual Absolute Risk of Esophageal Adenocarcinoma: Moving towards Tailored Screening and Prevention. Int. J. Cancer doi:10.1002/ijc.29988 (2016).
Ross-Innes CS, et al. Risk stratification of Barrett’s oesophagus using a non-endoscopic sampling method coupled with a biomarker panel: a cohort study. Lancet Gastroenterol Hepatol 2, 23–31 (2017).
The National Cancer Institute maintains a site devoted to cancer risk models: https://epi.grants.cancer.gov/cancer_risk_prediction/